New Model of Mental Health Care with Promising Early Results
Jay Getten | Oct 17, 2022 | 6 min read
Background
Montana has ranked among the top five states with the highest suicide rates for over 40 years and in 2018, Montana ranked third highest, based on per capita suicide death rate of 24.6 deaths per 100,000 people. Additionally, over the past decade the rate of suicide in Montana has been nearly double the national rate (DPHHSMT, 2020). One in five Montanans report living with a depressive disorder or experiencing a depressive episode. While 20% of adults in Montana report binge drinking compared to 16% nationally (Loveland, 2016).
In rural states like Montana every part of the mental health system has been stretched beyond capacity during the pandemic (Lutey, 2021). Currently there are over twenty geographic areas experiencing behavioral health provider shortages. Health systems do not have the ability to meet the immense increase in need and address declining workforce issues (Durkin, 2021).
New Model of Care
New systems are required for early detection of risk factors and new models of mental healthcare are needed to address the current mental health crisis and reduce suicidality. Behavioral Health Consulting Solutions (BHCS) has developed a new model of care to attempt to meet the growing mental health needs and workforce shortages. Our model of care that we are calling an integrated information model (IIM) for lack of a better term has shown promising early results. The following section summarizes our approach.
IIM
- A curiosity to dive deeper and not just accept difficulties at face value. Also, a desire to connect disparate pieces of information to find missing or overlooked pieces to the larger picture that is our patients lives.
- Exploring current peer-reviewed research to ensure we understand and keep up with evolving best practices. Utilizing the research to discover connections between mental health conditions and physical health comorbidities to recognize the interplay between them.
- Maximizing health information technology to align with the United States Preventive Services Task Force's recommendation of best practice screening for mental health conditions to ensure accurate diagnosis, effective treatment, and appropriate follow-up care (Jeffrey et al., 2021).
- Our proprietary Seidr clinical decision support system (CDSS) software allows us to effectively apply a bundled assessment approach that screens for multiple mental health conditions individually. One of our team members described the system as “labs for mental health” because of how it is like a comprehensive panel assessing for each condition individually.
- The triaging feature helps our practice to identify level of patient acuity which allows our team to quickly schedule high risk patients before they experience a crisis.
- The system's diagnostic feature which includes lines of questioning from the DSM-5 and ICD-11 which have been modified so that are easy for patients to understand. This allows our clinicians to blend quantitative assessment tool data with how patients experience specific diagnostic criteria in their lives.
- Seidr's tracking feature assists our team with following up with patients to ensure they are responding to treatment and helps us determine if we need to explore a different diagnosis or treatment.
- Seidr is currently in the beta testing phase and if it continues to show results BHCS plans to market the CDSS system to providers in March 2023.
- Adapting precision health care to mental health practice by synthesizing current research, quantitative data, clinical expertise, and patient experience as well as communicating our analysis in a way that is relatable to our patients.
- Precision health care focuses on predicting future outcomes in patients with health conditions or risks for negative outcomes and indicates the best treatment approach for specific conditions to enhance individual treatment outcomes (Lutz et al., 2022).
- Services are time limited. Everything we do is to foster patient independence, increase functioning, and work towards graduation from treatment.
Early Results
Though our organization is less than a year old, our patient outcomes have been startling. We have measured pre and post assessment/treatment patient depression and anxiety outcomes utilizing Patient Health Questionnaire 9 (PHQ-9) and Generalized Anxiety Disorder 7 (GAD-7).
- The PHQ-9 is a self-administered depression module screening tool. It contains 9 questions that help identify patients with symptoms of depression. Patient responses are scored 0-3 and has a total score range of 0-27. The PHQ-9 scoring indicates level of severity: 1-4 minimal depression, 5-9 mild depression, 10-14 moderate depression, 15-19 moderately severe depression, and 20-27 severe depression.
- The GAD-7 scale is self-report tool for assessing anxiety. Patients to rate each of the seven items on a four-point scale from 0-3 and the score can range from 0 to 21. The GAD-7 scoring ranges indicate level of severity: 0-4 minimal anxiety, 5-9 mild anxiety, 10-14 moderate anxiety, and 15-21 severe anxiety.
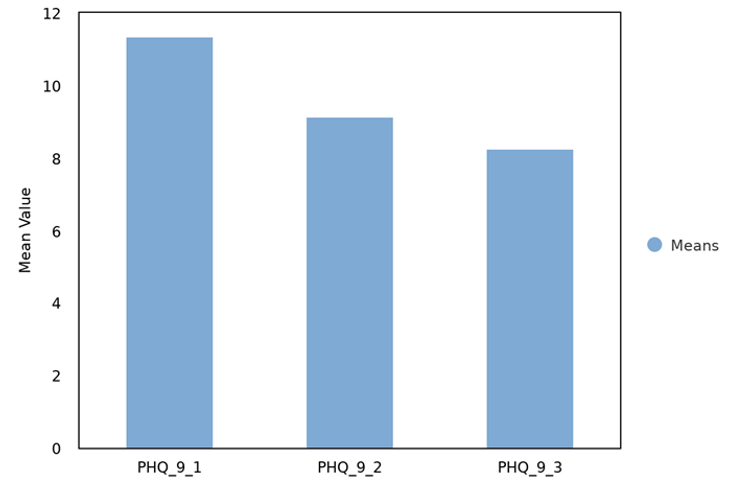
Out of a sample of 129 BHCS patients who completed an initial follow-up assessment saw an average decrease in PHQ-9 scores by over 2 points (11.36 to 9.16). A sample of 52 patients who completed an additional follow up assessment saw an average decrease in PHQ-9 scores by over 3 points (11.36 to 8.27).
A sample of 128 patients who completed an initial follow-up assessment saw an average decrease in GAD-7 scores by nearly 3 points (10.17 to 7.87). A sample of 52 patients who completed an extra follow up assessment saw an average decrease in GAD-7 scores by over 3 points (10.17 to 6.94).
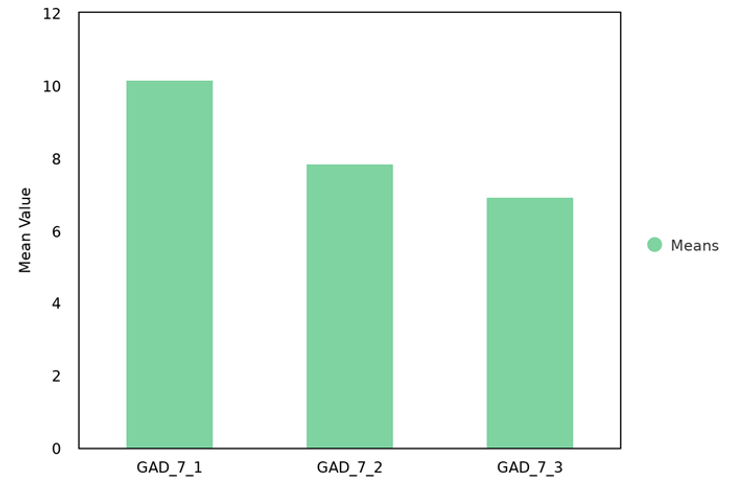
A two to three average decrease in scores may not seem like much. However, the 2-3 decrease in both assessment tools indicates that on average our patients have moved from moderate to mild depression and anxiety symptoms. Though promising we know that more time and information are needed before we can say that our approach is validated. Plus, our foundation of curiosity will not let us rest on early successes because we can always dive deeper.
References
DPHHSMT. (2020). Survivors of suicide loss, 2018 [PDF]. Montana.Gov. Link
Durkin, E. (2021). The US's ‘second pandemic': Surges in behavioral-health needs. National Journal. Link
Jeffrey, J., Do, M.-C. T., Hajal, N., Lin, Y.-H., Linonis, R., Grossman, M. S., & Lester, P. E. (2021). Using web-based technology to improve depression screening in primary care settings. BMJ Open Quality, 10(1), e001028. Link
Loveland, K. (2016). Integrated behavioral health in montana: A baseline assessment of benefits, challenges, and opportunities. Link
Lutey, T. (2021, May 12). Montana mental health situation worsened by covid-19, expert says. Billings Gazette. Link